Abstract
Background: Treatment advances, such as all-trans retinoic acid, have improved outcomes in acute promyelocytic leukemia (APL), but early mortality (defined here as death ≤7 and <30 days from diagnosis) continues to be a barrier to improving overall survival, especially in older patients. Few population-based studies have evaluated the impact of complications on early mortality by age in APL patients.
Methods: Using a retrospective observational study design, we analyzed linked data from the California Cancer Registry and hospital discharge records in California from 1999-2014. We identified patients ≥15 years of age diagnosed with APL who were hospitalized within 30 days of diagnosis (N =980). Multivariable logistic regression analyses were used to determine the association of complications with early mortality (overall and by age group), adjusting for sociodemographic factors, comorbidities and hospital type. Results are presented as adjusted odds ratios (OR) and 95% confidence intervals (CI).
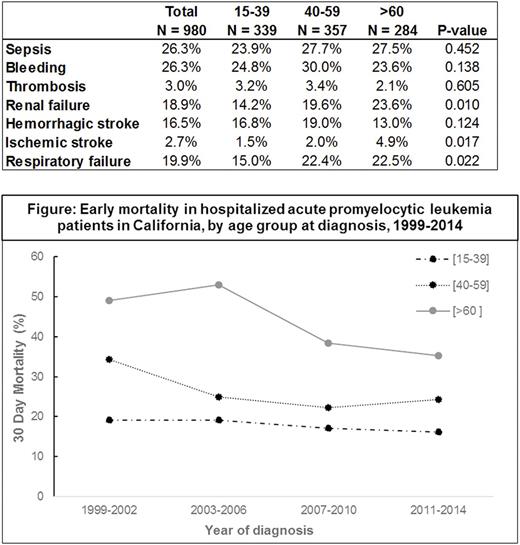
Results: Of 980 patients hospitalized with APL, 17.0% (n=167) died in the first 7 days and 28.0% (n=274) died within 30 days of diagnosis. 7-day mortality decreased over time (19.7%, 1999-2002; 14.3%, 2011-2014). There was consistent positive association of 7-day mortality with increasing age (12.4%, 15-39 years, 17.1%, 40-59 years, and 22.5%, >60 years). Major complications in those that died at 7 days included bleeding, hemorrhagic stroke and respiratory failure, with significantly higher rates of bleeding and hemorrhagic stroke seen in those aged 15-39 compared with those >60 years. 30-day mortality also decreased over time (33.2%, 1999-2002; 24.8%, 2011-2014), with a positive association with increasing age (17.7%, 15-39 years, 25.8%, 40-59 years, and 43.0%, >60 years). (Figure) Complications did not vary substantially by age, except that older patients (>60 years) had higher rates of ischemic stroke, renal failure and respiratory failure than those aged 15-39. (Table) In multivariable models, major bleeding (OR 2.13, CI 1.20-3.78), hemorrhagic stroke (OR 5.48, CI 2.78-10.80), renal failure (OR 1.88, CI 1.18-2.99), and respiratory failure (OR 7.82, CI 4.89-12.52) were associated with 30-day mortality. Higher 30-day mortality also was associated with older age (>60 vs 15-59 years) and having >3 comorbidities (vs 0). Race/ethnicity, marital status, neighborhood socioeconomic status, health insurance and hospital type was not significantly associated with early mortality.
Conclusions: Almost one third of APL patients die within 30 days of diagnosis, the majority within the first 7 days, with older patients having the highest 30-day mortality. Complications of bleeding, hemorrhagic stroke and respiratory failure continue to drive early mortality, but socioeconomic factors and hospital type did not impact early mortality. Because early mortality, not drug resistance, continues to be a major cause of treatment failure in APL patients, more robust initiatives to address these complications, including more aggressive supportive measures and universal prophylaxis of differentiation syndrome, may lead to better outcomes.
Jonas: AbbVie, Celgene, Daiichi Sankyo, Pharmacyclics, Genentech/Roche, Glycomimetics, Esanex, Kalobios: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees; Rigel: Consultancy. Wun: Janssen: Other: Study steering committee and research support (site PI); Pfizer: Other: Study steering committee and research support (site PI).
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal